Vagus nerve stimulation (VNS) has emerged as a promising intervention for various health conditions, from depression to epilepsy. By sending mild electrical signals to the vagus nerve through a small device, VNS can manage symptoms and improve quality of life. The popularity of this treatment modality has led to the development of numerous devices, each claiming to offer unique benefits and features. Finding the best VNS device means evaluating efficacy, user-friendliness, and potential impacts on one’s health.

As someone eager to enhance their wellbeing through non-invasive techniques, I understand the criticality of making an informed decision when selecting a VNS device. Whether one seeks to alleviate mental health challenges or address chronic pain, the device chosen should align with specific needs and lifestyle considerations. With advancements in technology, devices now range from wearable units to implantable systems, making it crucial to comprehend the differences and pinpoint the most fitting option for an individual’s circumstances.
Key Takeaways
- Identifying the top VNS device requires assessing its effectiveness and usability.
- An informed choice stems from understanding one’s own health needs and device specifications.
- Technological advancements offer various VNS options, from non-invasive to implantable devices.
Understanding Vagus Nerve Stimulation
The vagus nerve is the tenth cranial nerve and a pivotal element of the autonomic nervous system, influencing the heart, digestion, and mood. Vagus Nerve Stimulation (VNS) is a treatment involving the use of a device to send electrical impulses to this nerve.
VNS functions by intermittently stimulating the vagus nerve with electrical signals. I understand this is particularly beneficial for:
- Controlling seizures in epilepsy when other treatments are ineffective
- Managing treatment-resistant depression, offering an alternative when conventional therapies don’t work
The therapy is administered using a small device, similar to a pacemaker, which is implanted under the skin, typically in the chest area. Wires from the device are connected to the left branch of the vagus nerve.
Clinical trials and studies have evidenced VNS as a promising treatment for certain conditions. For instance:
- Patients with epilepsy may experience a reduction in seizure frequency.
- Those struggling with depression often report improvements in mood.
However, there’s a risk spectrum associated with any intervention. Complications can include:
- Hoarseness
- Shortness of breath
- Discomfort at the site of stimulation
Neuromodulation, the umbrella under which VNS falls, targets the nervous system to modulate its activity. In this context, VNS helps balance the equilibrium between the sympathetic and parasympathetic systems, often leading to:
- Stabilized heart rate
- Alleviated inflammatory responses, which can mitigate pain
In conclusion, VNS has carved a niche as a valuable tool against certain health conditions where other therapies have fallen short. It emphasizes the interconnectivity between our nervous system and overall well-being.
Types of Vagus Nerve Stimulators
In this section, I will discuss the two primary types of vagus nerve stimulators: implantable and noninvasive devices. Each type is distinct in its application and operation, catering to different patient needs.
Implantable Vagus Nerve Stimulators
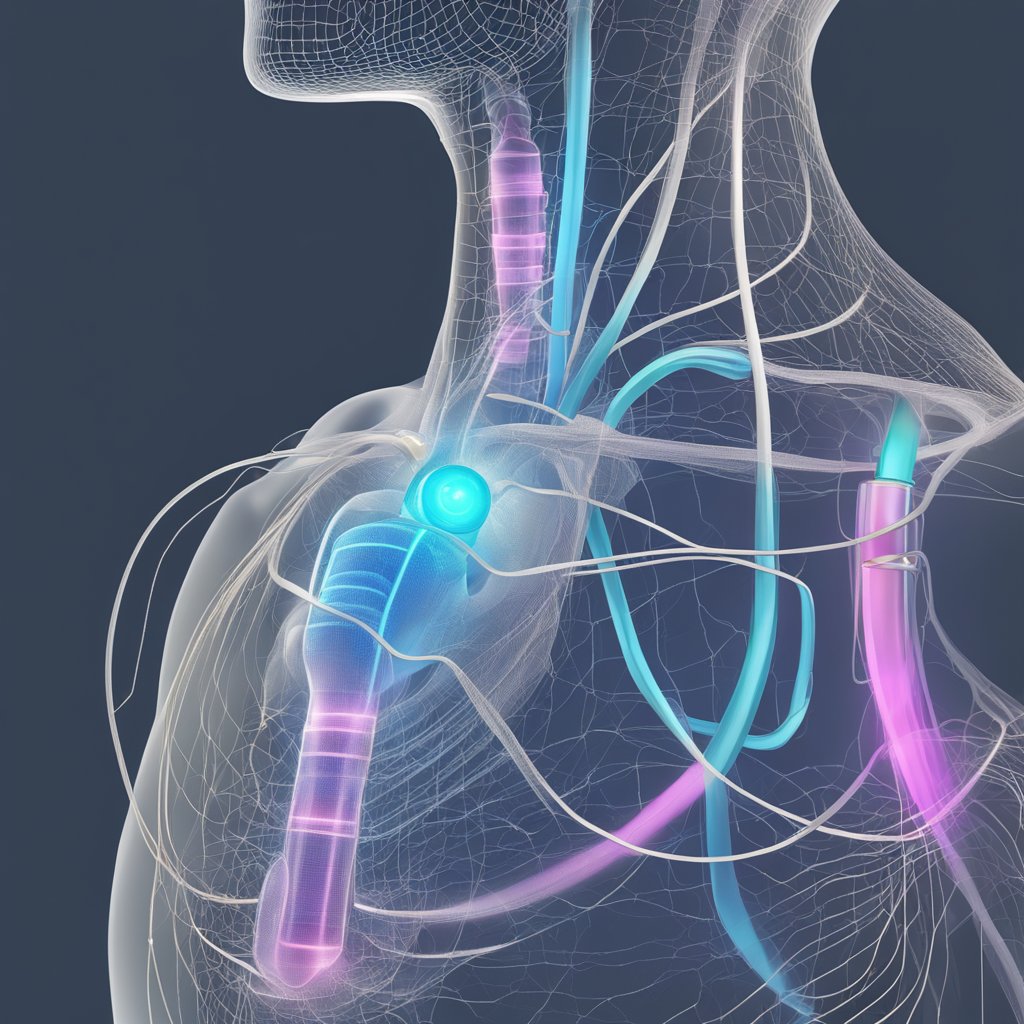
Implantable vagus nerve stimulators function similarly to a pacemaker. They are small devices featuring a battery-powered pulse generator, which is implanted under the skin in the chest through a surgical procedure. The generator is then connected to the vagus nerve through leads—thin insulated wires. These devices emit electrical signals to stimulate the vagus nerve with the aim of treating various health conditions.
The implantation requires anesthesia and an incision in the neck to attach the leads to the vagus nerve, and another in the chest or abdomen to place the pulse generator. The vagus nerve stimulator’s settings are programmable, allowing physicians to adjust the strength and timing of the electrical impulses. Patients should be aware of some potential side effects, such as a tingling sensation or throat discomfort during the stimulation.
- MRI compatibility: Most contemporary implantable devices are compatible with magnetic resonance imaging (MRI), but it’s vital to confirm this with the manufacturer.
- FDA approval: Implantable vagus nerve stimulators have been approved by the Food and Drug Administration (FDA) for the treatment of epilepsy and depression.
Noninvasive Vagus Nerve Stimulators
Noninvasive vagus nerve stimulation (nVNS) devices, also known as transcutaneous vagus nerve stimulation (tVNS) gadgets, offer a less invasive option. These devices stimulate the vagus nerve without the need for surgery. Instead, they deliver electrical impulses through the skin to accessible vagus nerve branches, typically in the neck or the ear.
Types of nVNS devices include:
- Handheld Stimulators: Patients place these devices against the skin to deliver timed electrical pulses.
- Ear Clip Stimulators: These devices attach to the ear, targeting the vagus nerve endings located there.
Noninvasive stimulators are battery-operated and often programmable, giving users the flexibility to control the intensity and duration of the stimulation. Side effects tend to be minimal, with some users reporting mild tingling or headaches.
Given their noninvasive nature, these devices are typically more accessible and do not require the same level of medical intervention as implantable stimulators. FDA clearance for nVNS devices varies based on their intended use and the specific device.
Considerations and Potential Side Effects
Choosing the right vagus nerve stimulation (VNS) device is crucial, as it not only affects the level of symptom relief but also determines the potential side effects and medical considerations one may face. In making an informed decision, understanding the risks and required post-operative care is essential.
Medical and Surgical Considerations
In assessing VNS devices, I consider the invasiveness of the surgery and the implications of having a foreign body implanted. Implantation entails a surgical procedure that carries risks such as infection and inflammation. Post-operative recovery also requires attention, as the body adjusts to the implant. Meticulous handling of the device pre and post-surgery minimizes these risks. Managing chronic conditions like migraines and cluster headaches could involve adjusting the device settings, a process that should be straightforward and accessible.
Disorders such as stroke could potentially complicate the implantation process. Therefore, thorough pre-surgical evaluations are vital. Beyond the initial surgery, long-term aspects such as the durability of the device and the ease of battery replacement are also critical factors.
Side Effects and Risks
VNS therapy’s side effects are usually mild but can include hoarseness, cough, and difficulty swallowing due to the device’s proximity to the vocal cords. While some individuals may experience transient symptoms, others might face persistent issues like vocal cord paralysis. Incidence of these side effects:
- Hoarseness: Common after activation, often temporary
- Cough: Can occur during stimulation
- Difficulty Swallowing: Infrequent but may happen after implantation
More severe risks, although rare, can entail complications leading to additional medical intervention. It’s important to understand these risks to balance the potential benefits with the drawbacks. VNS for headaches or migraine may trigger or exacerbate symptoms in some individuals, hence personalized programming of the device is paramount.
Lastly, I look at potential effects of device removal, whether due to infection or device failure. This should be a structured process to safeguard against further complications. My choices are informed by comprehensive data on both the efficacy and safety of VNS devices.
Improving Life with Vagus Nerve Stimulators
Vagus nerve stimulators have emerged as a significant tool in enhancing therapeutic outcomes for various chronic conditions, directly impacting lifestyle and wellness. These devices are a beacon of hope for those seeking alternatives to conventional treatments.
Enhancing Treatment for Chronic Conditions
Epilepsy: My research indicates that vagus nerve stimulators can reduce seizure frequency, benefiting epilepsy patients. With regular use, quality of life has improved as VNS therapy helps to manage and mitigate seizures.
Depression and Mood: The stimulators also offer an adjunct therapy for depression, with some patients experiencing mood stabilization. Their efficacy in modulating emotional well-being is a crucial aspect of my findings.
Chronic Pain: Regarding pain management, these devices have shown promise. Individuals with conditions like rheumatoid arthritis have reported reduced pain levels, facilitating better rehabilitation outcomes.
Inflammatory Bowel Disease and Digestive System: For inflammatory bowel disease, vagus nerve stimulation appears to help in regulating the digestive system, leading to a decrease in the frequency and severity of symptoms.
Lifestyle and Vagus Nerve Stimulation
Exercise and Stress: In my experience, incorporating VNS devices with routine exercise can amplify stress reduction benefits. This is especially pertinent for managing conditions like anxiety and potentially Alzheimer’s disease.
Heart Rate and Blood Pressure: By monitoring and adjusting stimulation parameters, these devices can contribute to stabilizing heart rate and blood pressure, indicative of stress relief.
Sleep Apnea and Wake Up Quality: Sleep patterns are critical to my overall well-being, and the VNS has shown potential in improving symptoms of sleep apnea, affecting how I wake up more refreshed.
Deep Breathing, Yoga, and Music: As a proponent of holistic therapy, I integrate deep breathing, yoga, and soothing music with VNS to enhance the calming effects, which has substantially benefited my quality of life.
Frequently Asked Questions
In my research, I’ve focused on the crucial aspects of vagus nerve stimulation devices to address common inquiries clearly and factually.
What are the benefits of using a vagus nerve stimulation device?
Vagus nerve stimulation (VNS) devices have been shown to offer several benefits, including reducing the frequency of seizures in epilepsy and alleviating symptoms of depression. Some studies suggest that VNS can also improve quality of life for individuals with treatment-resistant depression.
How can I safely use a vagus nerve stimulation device at home?
To safely use a VNS device at home, it’s important to follow the manufacturer’s instructions carefully. I only use the device as prescribed by a healthcare provider and ensure that I’m trained on the correct placement and usage.
What features should I look for in a high-quality non-invasive vagus nerve stimulator?
In a high-quality non-invasive vagus nerve stimulator, I would look for features like adjustable intensity settings, a timer for tracking therapy duration, a comfortable ergonomic design, and FDA approval to ensure the device has been tested for safety and efficacy.
Can non-invasive ear clip vagus nerve stimulators provide effective results?
Yes, non-invasive ear clip vagus nerve stimulators can provide effective results for certain conditions. Clinical studies support their use in treating conditions such as migraines and episodic cluster headaches by targeting the auricular branch of the vagus nerve.
What are the differences between invasive and non-invasive vagus nerve stimulators?
The primary difference is that invasive stimulators require surgical implantation while non-invasive ones do not. Invasive VNS devices usually have a pulse generator implanted in the chest with leads connected to the neck’s vagus nerve. Non-invasive devices are applied externally and can be used on-demand.
How do health professionals rate the effectiveness of vagus nerve stimulation devices?
Health professionals typically rate the effectiveness of vagus nerve stimulation devices based on clinical trial data, patient outcomes, and their experience with individual cases. Positive improvements in conditions like epilepsy and depression have led to many in the medical community supporting their therapeutic benefit.