Experiencing sternum pain can be disconcerting given its proximity to the heart and lungs, leading many to fear a serious issue. The sternum, or breastbone, is located in the center of the chest, and its function is integral to the rib cage, as it helps protect vital organs such as the heart and lungs. When sternum pain occurs, it may feel like a sharp, aching, or pressure sensation that can worsen with deep breaths or coughing.
Various factors can lead to this discomfort, ranging from muscular strain to more serious cardiac conditions. It is critical to consider the nature of the symptom—whether it’s acute or chronic—and the presence of accompanying symptoms like difficulty breathing. For some, it may occur after physical exertion or an injury, while in others, it might be a sign of an underlying medical condition that requires prompt attention.
Seeking medical advice for sternum pain is important for accurate diagnosis and timely treatment. Healthcare professionals will generally conduct a thorough evaluation, including a physical examination and potentially imaging studies, to determine the root cause. Once identified, the treatment options can vary, from conservative management with rest and pain relief to more targeted therapies for underlying causes.
Key Takeaways
- Sternum pain, often felt as a sharp or aching sensation, is important to monitor due to its potential underlying causes.
- Accurate diagnosis is essential and may involve examination and imaging to identify the source of discomfort.
- Treatment varies depending on the cause, but it is aimed at pain management and addressing any underlying issues.
Anatomy of the Sternum
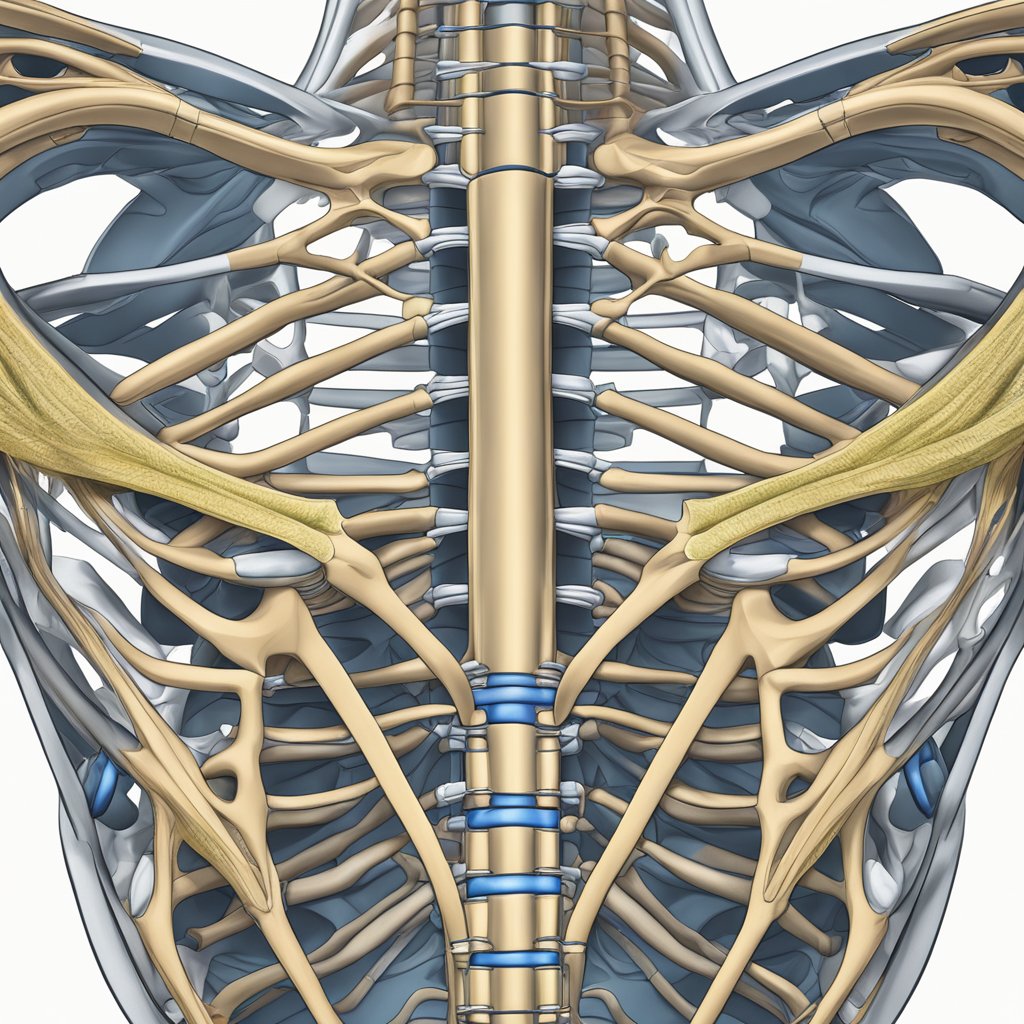
The sternum, commonly known as the breastbone, is central to the structural integrity of my chest, protecting vital organs such as my heart and lungs.
Components and Function of the Sternum
Structure: My sternum is a flat, dagger-shaped bone located in the center of my chest. It consists of three parts:
- Manubrium: The upper section that articulates with the clavicles (collarbones).
- Body (Gladiolus): The longest part of the sternum, it connects to the majority of my ribs via costal cartilage.
- Xiphoid Process: A small, cartilaginous projection at the lower end, which ossifies (becomes bone) as I age.
Function: As a key component of my rib cage, the sternum provides attachment points for several muscles involved in breathing and serves as a protective shield for my heart and lungs.
Connection to Ribs and Collarbones
- Ribs: My sternum connects to my ribs via strips of hyaline cartilage known as costal cartilage. This forms part of the costosternal joints, which attach the first seven pairs of ribs (true ribs) directly to my sternum.
- Clavicles: The manubrium of my sternum forms the sternoclavicular joint with my clavicles. This joint facilitates the range of motion of my shoulders and arms.
Common Causes of Sternum Pain
In my experience, sternum pain can originate from various medical conditions that affect the chest area. The pain might range from mild discomfort to severe and is often an indication of underlying issues that need medical evaluation.
Musculoskeletal Disorders
Costochondritis: This is an inflammation of the cartilage connecting the ribs to the sternum, often causing sharp pain. It’s usually a result of physical strain or injury.
Muscular Strain or Bruise: Sternocleidomastoid and pectoral muscles can be strained during physical activities, leading to sternum pain.
Fracture: Direct trauma to the chest can fracture the sternum, resulting in severe, acute pain.
Tietze Syndrome: Similar to costochondritis but with noticeable swelling, this rare condition can cause localized pain at the costosternal joint.
Respiratory Conditions
Pneumonia: An infection that inflames air sacs in one or both lungs can manifest with sternum pain when coughing or breathing deeply.
Pleurisy: This condition involves inflammation of the tissues that line the lungs and chest cavity, which can cause sharp chest pain that worsens with breathing.
Cardiac Concerns
Heart Attack: A blockage of blood flow to the heart can result in pain centralized in the sternum, which may spread to the arms, neck, or jaw.
Gastroesophageal Reflux Disease (GERD): Though not directly associated with the heart, acid reflux can create a burning sensation behind the sternum.
When experiencing persistent sternum pain, it’s crucial to seek medical attention as some of these conditions require prompt treatment.
Diagnosing Sternum Pain
When I experience sternum pain, it’s important for me to know that accurate diagnosis is key to determining the right treatment. The diagnostic process typically involves two main approaches: a physical examination and various imaging and tests.
Physical Examination
During the physical examination, my doctor will ask me detailed questions about my sternum pain, such as its location, intensity, duration, and any associated symptoms. They will also need to know about any recent injuries or activities that may have contributed to my pain. This conversation helps them rule out or consider potential causes of sternum pain. The physical exam includes palpating the area to check for tenderness or abnormalities.
-
Questions About Pain:
- Location
- Intensity
- Duration
-
Associated Symptoms: (shortness of breath, palpitations, etc.)
-
Recent Injuries/Activities: (asked to determine possible causes)
Imaging and Tests
If the cause of my sternum pain isn’t clear from the physical exam, my doctor may order further imaging and tests. These can confirm or rule out certain diagnoses and may include:
- Chest X-ray: To look at the structures of the chest and the integrity of the sternum.
- Electrocardiogram (EKG/ECG): To check for heart attack symptoms or other heart-related issues.
- Echocardiogram: To view the heart’s motion and structure.
- Blood tests: To look for markers of inflammation or damage that could be causing the pain.
| Test Type | Purpose |
|---|---|
| Chest X-ray | Examines chest structure and sternum integrity. |
| EKG/ECG | Checks for heart-related issues. |
| Echocardiogram | Assesses heart motion and structure. |
| Blood tests | Identifies markers of inflammation or damage. |
It’s crucial that I seek immediate medical attention if the pain is severe, sudden, or accompanied by symptoms such as difficulty breathing or pressure in the chest, as these could indicate a potential heart attack or other emergency conditions. My doctor will determine the necessity for these tests based on my specific symptoms and the findings from the physical exam.
Treatment and Management
When addressing sternum pain, it’s crucial to identify the appropriate course of action, which may include immediate remedies, standardized medical interventions, and a structured recovery process.
Immediate Remedies
For immediate relief of sternum pain, I recommend applying ice to the affected area to reduce inflammation and tenderness. Rest is also imperative to prevent further injury, especially if the pain is due to an acute injury like a sternoclavicular joint injury or collarbone fractures.
- Ice: Apply for 15-20 minutes every hour as needed.
- Rest: Avoid activities that exacerbate pain.
Medical Interventions
Should the sternum pain be severe or persistent, I advise seeking medical attention for a proper diagnosis and treatment plan. Treatment may involve:
- Medication: Over-the-counter pain relievers or prescription pain medication.
- Steroid injections: To reduce inflammation in chronic pain cases or specific injuries.
- Surgery: A last-resort option for serious conditions such as complicated fractures or injuries that do not heal with conservative treatment.
Recovery and Rehabilitation
The path to regain full function involves comprehensive recovery and rehabilitation strategies:
- Physical therapy: to rebuild strength and flexibility.
- Guided rest: strategized periods of rest to facilitate healing without allowing joint stiffness or muscle atrophy.
| Phase | Strategy |
|---|---|
| Acute Recovery | Rest and immobilization as necessary |
| Rehabilitation | Gradual increase in physical therapy |
| Long-term | Routine strengthening exercises |
It’s important to follow the advice of healthcare professionals throughout the recovery process to avoid the recurrence of pain.
Frequently Asked Questions
Understanding sternum pain is important, as it can be a symptom of various conditions, some benign and others requiring immediate attention. Below are answers to common queries related to sternum discomfort.
What are common causes of pain in the center of the chest between the breasts?
My investigation into this matter reveals that sternum pain centrally located can be due to costochondritis, muscle strain, injury, or underlying cardiac conditions. It’s imperative to assess the pain carefully to determine its cause.
How can I alleviate discomfort in the sternum after sleeping?
I suggest adjusting sleeping positions and investing in a supportive mattress and pillows to reduce sternum discomfort after sleeping. If the pain persists, it’s advisable to consult a healthcare professional for a tailored approach.
Is it normal to experience sternum pain when engaged in deep breathing?
It is not uncommon to feel pain in the sternum during deep breathing, especially if conditions like costochondritis or inflammation are present. Yet, persistent pain warrants a more thorough medical evaluation to exclude serious issues.
Could acid reflux be responsible for pain near the sternum area?
Yes, acid reflux can cause pain near the sternum, often described as heartburn. This pain typically arises from stomach acid irritating the esophagus and can be quite discomforting.
What might be the reason for sternum pain paired with back pain?
When sternum pain is accompanied by back pain, potential causes could include musculoskeletal issues, such as poor posture or vertebral problems, as well as referred pain from cardiac or gastrointestinal conditions.
Are there specific stretches I should avoid to prevent pain in the sternum?
To prevent sternum pain, I must caution against overstretching or performing high-impact exercises that place excessive pressure on the chest area. Gentle stretches, with attention to proper form, may minimize the risk of pain.